What We Treat
Gastrointestinal Cancer Specialist Melbourne




About Gastrointestinal (GI) Cancer
Gastrointestinal (GI) cancers can affect the digestive tract and the organs that support digestion, including the oesophagus, stomach, bowels, pancreas, liver, and rectum.
Cancer in these organs may impact vital functions such as eating, swallowing and absorbing nutrients, and can have a strong impact on your daily life and overall health.
Radiation therapy may be included in the treatment of several forms of gastrointestinal cancers, either as a primary treatment, in combination with chemotherapy or surgery, or to help manage symptoms.
Radiation therapy may be used for:
- Stomach Cancer (gastric cancer) develops from abnormal cell growth in the lining of the stomach. Symptoms may include indigestion, heartburn, difficulty swallowing, weight loss and bloating. Radiation therapy may be used alone or in combination with chemotherapy to potentially shrink tumours before surgery, or as adjuvant after surgery. It may also be used for symptom control, aiming to reduce pain, bleeding or difficulty swallowing.
- Oesophageal Cancer develops in the tube that carries food from the mouth to the stomach. It is slow growing and my not exhibit symptoms until it reaches an advanced stage. The two main types of oesophageal cancer are adenocarcinoma (more common in Australia) which affects the lower part of the oesophagus, and squamous cell carcinoma, found in the upper section. Radiation therapy may be considered as a primary treatment with chemotherapy for squamous cell carcinoma and in certain cases of adenocarcinoma before or after surgery.
- Rectal and Bowel Cancer affects the large intestine or rectum and is among the most common cancers in Australia. Symptoms may include changes in bowel habits, blood in the stool, abdominal pain and unexplained weight loss, and early detection may significantly increase the success of treatment. Radiotherapy is most often used in rectal cancer, most commonly before surgery. It can also be used as part of a primary treatment plan in combination with chemotherapy (TNT: Total Neoadjuvant Treatment). Radiation therapy may sometimes be considered for bowel cancers using specialised techniques.
- Pancreatic Cancer occurs in the pancreas, an organ in the abdomen that helps with digestion and hormone production. Pancreatic cancer can spread quickly and is often diagnosed late due to the absence of symptoms in the early stages. Radiation therapy can be used as part of radical treatment using fractionated EBRT, stereotactic radiation, or more advanced CyberKnife technology in certain cases.
- Liver Cancer includes primary cancers such as hepatocellular carcinoma (HCC), which begin in the liver, as well as secondary cancers that have spread from other parts of the body. Radiation therapy may be used to treat both HCC and metastatic disease within the liver, by using EBRT machine, stereotactic radiation therapy, or Cyberknife technology.
- Anal Carcinoma is a type of squamous cell carcinoma that develops in the tissues of the anus. It may present with symptoms such as bleeding, pain, or changes in bowel movements. Radiation therapy is commonly used as a primary treatment, often in combination with chemotherapy, and may also be considered in advanced cases to help relieve symptoms and improve comfort.
Radiation Therapy for Gastrointestinal Cancer Treatment
Treatment for gastrointestinal cancers often draw on several different approaches which may leave you feeling confused or uncertain. If you or someone close to you is navigating a cancer diagnosis, understanding the treatment options available can help you feel more informed and supported.
Radiation therapy is often considered as part of a treatment plan for gastrointestinal cancers. It can be used as part of a neoadjuvant (before surgery) or adjuvant (after surgery) approach, aiming to shrink tumours or kill remaining cancer cells. It may also be used along with chemotherapy as a primary standalone treatment option, or with the goal of reducing symptoms such as bleeding, pain or difficulty swallowing.
Different types of radiation therapy may be used in gastrointestinal cancers, including:
Stereotactic radiation therapy (SRT), also referred to as stereotactic ablative radiation therapy (SABR), is a focused form of radiation that delivers high doses to small, well-defined areas. Treatment is delivered with precise accuracy to minimise exposure to healthy tissue and organs. SBRT can be used in the treatment of primary and secondary tumours.
Superficial Radiation Therapy delivers low-energy radiation that penetrates only a few millimetres into the skin. It is a non-invasive approach that focuses on surface-level tumours without affecting deeper tissues. This makes it especially useful for treating non-melanoma skin cancers in sensitive areas such as the face, nose, or ears, where surgery may not be the best option.
CyberKnife is an advanced type of stereotactic radiation therapy that uses computer guided robotics and real-time imaging. This allows precise radiation to be delivered from multiple angles and adjusted for natural movement such as breathing during treatment. CyberKnife may be suitable for tumours in complex or hard-to-reach areas, including the prostate, lung, liver, pancreas, head and neck.
External Beam Radiation Therapy is one of the most common forms of radiation treatment. It uses a machine called a linear accelerator to direct beams of radiation from outside the body onto the cancer site. Up-to-date techniques such as Intensity-Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) allow the radiation dose to be shaped more precisely to the tumour, helping to protect surrounding healthy tissue. EBRT may be recommended for a wide range of cancers.
Your Treatment Journey
01
Referral
Your journey begins with a referral from your GP or specialist. This ensures we have the clinical information needed to assess your condition and plan the next steps in your care.
02
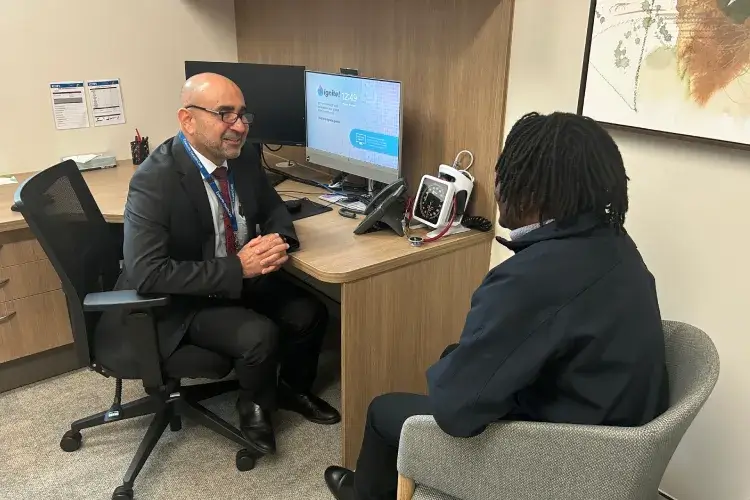
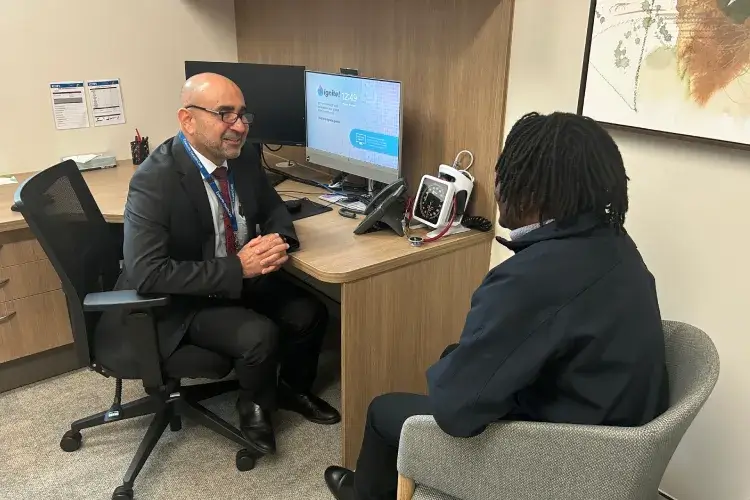
Initial Consultation and Treatment Plan
At your first appointment, you'll meet with our radiation oncologist Dr Mathlum to review your diagnosis and discuss treatment options. If radiation therapy is appropriate for you, we will outline a personalised treatment plan, so you know what to expect.
03
Treatment
Radiation therapy sessions are delivered at one of our Victorian clinic locations (depending on the type of radiation treatment you are undergoing). Our team will guide you through each session, monitoring your progress closely and answering any questions you may have about your treatment.
04
Post-Treatment Care
After your treatment plan has been completed, we'll provide follow-up appointments to check on your progress, help you manage any side effects and to continue to support your health and wellbeing.


Benefits of Radiation Therapy
- Comprehensive approach: Radiation therapy can be used as part of a comprehensive treatment plan, before or after surgery, or in combination with chemotherapy. We work with a team of specialists across multiple disciplines to determine the best overall treatment approach for each patient.
- Targeted precision: Advanced treatment approaches such as IMRT, VMAT and CyberKnife allow for highly accurate targeting of the cancer site while minimising damage to healthy surrounding tissues.
- Symptom management: Radiation therapy may help manage symptoms such as pain, bleeding, or difficulty swallowing in advanced GI cancers, contributing to improved comfort and quality of life.
- Shorter treatment sessions: Radiation is usually delivered as an outpatient service, meaning patients can attend an appointment and return home the same day.
- Medicare funding: Radiation oncology is funded by Medicare, covering up to 90% of treatment costs. If you are a Medicare card holder, you do not need private health insurance to access care through a private clinic.
Your GI Cancer Treatment Questions Answered
How is the radiation targeted to the tumour without damaging other tissue or organs?
What does a radiation session involve?
Can radiation therapy be used instead of surgery for GI cancers?
How many sessions of radiotherapy will I need?
How do I book an appointment?
Why Choose Us?


Experienced Specialist
Your care is led by Dr Maitham Mathlum, a radiation oncologist with more than 25 years of clinical experience, supported by a dedicated team who prioritise clear communication and patient support.
Advanced Technology
We provide access to modern radiation therapy techniques, including IMRT, VMAT, and CyberKnife, allowing treatment to be delivered with a high degree of precision and planning.
Personalised Treatment Planning
Every plan is tailored to the type and stage of cancer, as well as your overall health and individual circumstances. We work closely with your GP, specialists, and wider healthcare team to provide the best possible care.
Referrals from Practitioners
Radiation Oncologist
25 Years
Clinical Experience
Clinical Trials
Active Research
Training
Radiology Education


Take the Next Step in Your Treatment Journey
Every patient is unique, and so is every cancer treatment plan. If radiation therapy is being considered as part of your care, we will work with you and your doctors to explore the options most appropriate for your circumstances.
If you would like to learn more about whether radiation therapy may be suitable for your situation, speak with your GP or specialist about a referral, or contact our clinic for more information.

